Is Abdominal Pain After Sex a Warning Sign of a Vascular Disorder?
Abdominal pain after sex is a common issue experienced by both men and women, but 75% of women have experienced lower abdominal pain during or after sex at some point in their lifetime. The reasons for this discomfort can range from minor to severe, impacting your mental and physical health. Abdominal pain after sex can be challenging to discuss with your provider, but it can also indicate an underlying vascular disorder.
What Could Be Causing My Abdominal Pain?
Pain during or after sex can have non-vascular causes that typically resolve on their own but may sometimes require medical attention and prescribed medication. Urinary tract infections or sexually transmitted infections, for instance, need medical treatment. STIs can cause abdominal pain after sex for both men and women, but most non-viral STIs can be cured with antibiotics when detected early.
Other common, non-vascular causes for abdominal pain during and after sex include but aren’t limited to:
- Digestive issues such as irritable bowel syndrome, gas, constipation, or food intolerances
- Muscle strain, hernia, or other abdominal injury
- Stress, tension, and anxiety.
- Sexual positions
- Vaginal dryness
Listening to your body and communicating with your partner is the most effective way to approach health concerns like painful intercourse or abdominal pain after sex. While abdominal pain after sex is common for both men and women, women are at higher risk for underlying gynecological or vascular causes.
Your symptoms may be related to pelvic congestion syndrome if you’re experiencing abdominal pain after sex, chronic pelvic pain lasting six months or longer, painful intercourse, painful menstrual cycles, and frequent urination.
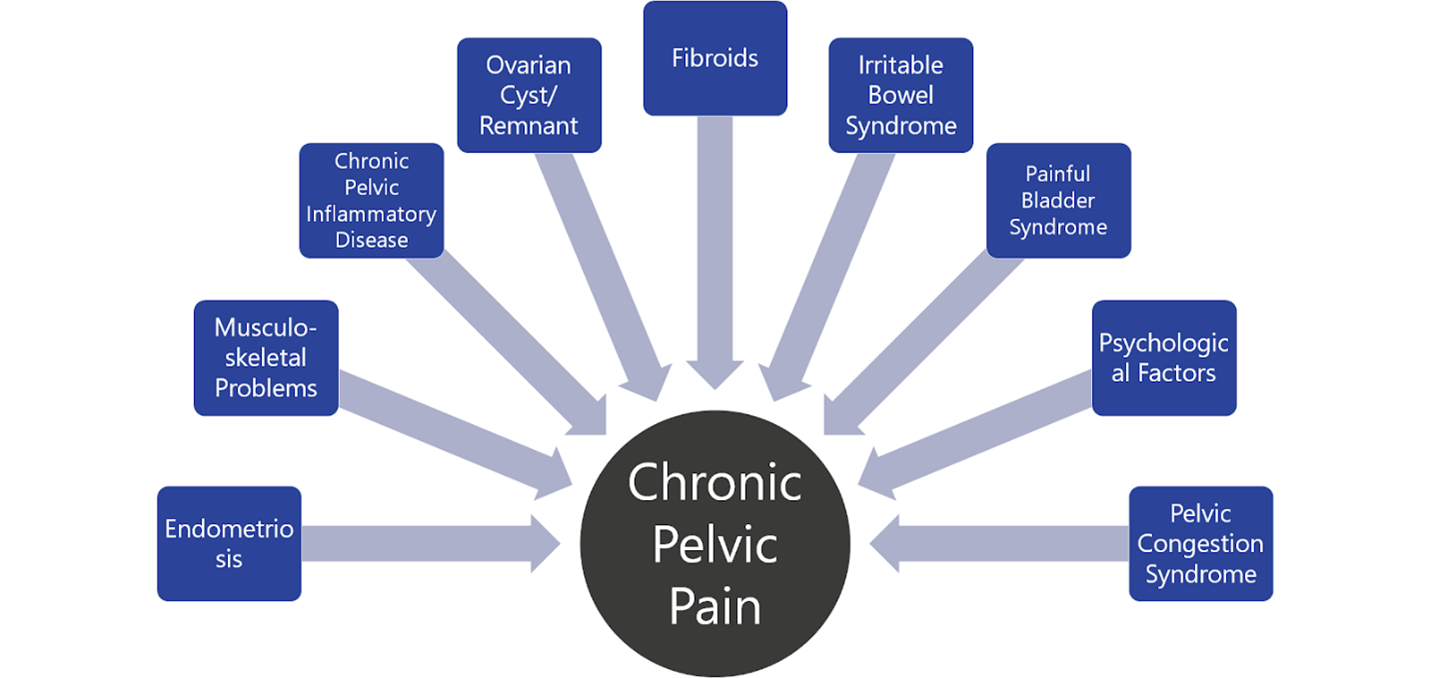
Before seeing a vascular specialist about your abdominal pain after sex, talk to your gynecologist or primary care provider to rule out gynecological causes of abdominal pain after or during sex, including:
- Uterine Fibroids
- Ovarian Cysts
- Pelvic Inflammatory Disease
- Endometriosis
- IUD (intrauterine device) placement
- Heavy Menstrual Periods
It might be time to consider consulting a vascular specialist regarding your pelvic pain if you have been experiencing persistent abdominal heaviness and chronic pelvic or abdominal pain and have already ruled out gynecological causes.
Could a Vascular Condition Like Pelvic Congestion Syndrome Be Causing My Pelvic Pain?
Pelvic Congestion Syndrome (PCS) is a vascular disorder that primarily affects women. Studies show that women are more likely to suffer from pelvic congestion syndrome than men, but men can also develop pelvic congestion syndrome.
Certain factors determine the risk of developing vascular disorders associated with pelvic pain, including:
- Hormone fluctuations
- Multiple pregnancies (2 or more)
- History of varicose veins or vascular problems
- Age
- Obesity
- Family history
- History of pelvic surgery or injury
Women who suffer from chronic pelvic pain lasting six months or more and experience painful menstrual cycles, painful intercourse, and frequent urination may be experiencing symptoms related to pelvic congestion syndrome. If you identify with these symptoms, you talk to your doctor about seeing a vascular specialist.
What Is Pelvic Congestion Syndrome?
Pelvic congestion syndrome is a vascular disorder that affects the veins in the pelvic region. These veins pump blood from the lower extremities back to the heart. When these veins don't function properly, they can become congested, causing pelvic venous insufficiency. This syndrome is commonly associated with leg pain and swelling.
Pelvic congestion syndrome can be complicated to diagnose and requires diagnosis and treatment by a vascular specialist. Underdiagnosis reflects the fact that women may experience pelvic and abdominal pain due to many other conditions, and the vascular component is often overlooked.
Because pelvic congestion syndrome is underdiagnosed and challenging, at Center for Vascular Medicine, we encourage patients struggling with symptoms of pelvic congestion syndrome to rule out any underlying gynecological conditions with their primary care provider or gynecologist before seeing a vascular specialist. This way, a gynecologist can rule out issues that may be at the root of pelvic pain, such as fibroids, endometriosis, or ovarian cysts.
Are My Symptoms Pelvic Congestion Syndrome?
Besides abdominal pain after sex, women with pelvic congestion syndrome tend to endure unusually painful menstrual cycles and painful intercourse. The discomfort can be exacerbated during a woman's day-to-day life while sitting or standing for an extended period. Common symptoms of pelvic congestion syndrome include but aren’t limited to:
Chronic Pelvic Pain: Chronic pelvic pain that does not respond to lifestyle changes or over-the-counter pain relievers is the most characteristic symptom, often described as a dull, aching pain that may sometimes become sharper. The pain typically persists for many months, worsens throughout the day, especially after standing long, and may improve when lying down.
Pain During or After Intercourse: Known medically as dyspareunia, this pain can be sharp or dull and may persist after intercourse.
Varicose Veins: Due to the dilation of veins, these may appear on the legs, vulva, or buttocks, similar to varicose veins that often occur in the legs.
Painful Menstruation: Menstrual cycles may become sore and can be associated with increased heaviness or irregular periods.
Backache and Leg Pain: Some individuals may experience lower back and leg aches.
Urinary Symptoms: Uncomfortable urinary symptoms, including increased frequency, urgency, or incontinence, can be symptoms of pelvic congestion syndrome.
Abdominal Bloating: Some women with PCS may experience feelings of heaviness or bloating in the pelvic area.
Unexplained Heavy or Painful Periods: Many symptoms, especially pelvic pain and heaviness, might worsen during menstrual periods due to increased blood flow and congestion in the pelvis.
According to John Hopkins Medicine, varicose veins are large, twisted veins typically developing on the legs. However, women with pelvic congestion syndrome can develop varicose veins in the vagina after pregnancy. When that occurs, varicose veins develop on the vulva, the labia majora, and the labia minora.
As many as one in ten pregnant women experience issues with veins in their pelvis. Commonly, these problems improve six to eight weeks after pregnancy. In some women, the veins stay and worsen with time and more pregnancies. The veins cause pelvic pain, itchy skin, painful vaginal intercourse, pelvic discomfort while walking, vulvar pressure, and a sense of swelling or heaviness.
Other signs and symptoms of pelvic congestion syndrome include pelvis pain that worsens during menstrual periods, dull, achy pains in the lower back, varicose veins on the buttocks or thighs, and bladder discomfort that makes it hard to control urination.
As most of these symptoms also align with other gynecological issues such as fibroids, endometriosis, and ovarian cysts, women struggling with pelvic congestion syndrome are often underdiagnosed or misdiagnosed.
What Causes Pelvic Congestion Syndrome?
Various factors, including physical and hormonal changes after pregnancy, can cause pelvic congestion syndrome. Iliac vein compression syndrome, also known as May-Thurner Syndrome, is a condition that can cause pelvic congestion syndrome.
May-Thurner Syndrome occurs when the iliac vein in the lower abdomen is externally compressed by the right common iliac artery, leading to vascular disorders throughout the leg, pelvic pain, and lower leg swelling. The pain usually worsens when standing or sitting for long periods and subsides when lying down.
Risk factors for developing pelvic congestion syndrome include but are not limited to:
Multiple Pregnancies: The most significant risk factor for PCS is multiple pregnancies, meaning more than two pregnancies. Pregnancy increases the blood volume in the body, which can pressure the veins in the pelvis, causing them to become dilated and varicose.
Hormonal Factors: Hormonal fluctuations, particularly those involving estrogen, can weaken the walls of veins, further contributing to their dilation.
Pelvic Varicose Veins: A hereditary predisposition to varicose veins increases the risk of developing varicosities in the pelvic region.
Lifestyle Factors: Lifestyles or careers that require long periods of sitting, standing, or other conditions that increase pressure on the pelvic region can exacerbate the risk of developing pelvic congestion syndrome.
Body Weight: Obesity or being overweight can also contribute to increased pressure on the pelvis, worsening the symptoms or risk of PCS.
A family history of varicose veins, especially in the legs or pelvis, may increase your risk of developing PCS.
How Will My Doctor Diagnose Pelvic Congestion Syndrome?
After you’ve worked with a primary care provider or gynecologist to eliminate any underlying gynecological or other medical conditions causing your pelvic pain, a vascular specialist will conduct tests to determine if you have pelvic congestion syndrome. Diagnosing pelvic congestion syndrome typically includes an ultrasound of the pelvic veins. For a more precise diagnosis, a venogram is often performed. This procedure involves injecting X-ray dye into the pelvic veins to make them visible during an X-ray, which is considered the most accurate method for diagnosing this condition.
How Is Pelvic Congestion Syndrome Treated?
Doctors usually tailor treatments to patients' specific underlying conditions. For pelvic congestion syndrome, some medical providers may prescribe starter medication. If symptoms do not improve with medication, the doctor may recommend other medical procedures.
Pelvic congestion syndrome (PCS) is treated using a combination of approaches, depending on the severity of symptoms and the patient's overall health. Here are some standard treatment options:
Medications: Pain relief is typically the first line of treatment, using over-the-counter or prescribed pain relievers. Hormonal therapies such as birth control pills or other hormonal manipulations may also be used to reduce congestion and pain.
Embolization: This is a minimally invasive procedure where a radiologist uses imaging guidance to block off the problematic veins contributing to the congestion. Embolization helps reduce pressure and pain. It's often considered an effective treatment for PCS.
Stenting: As the name suggests, PCS can be due to the obstruction or partial reduction of blood flow through the pelvis. A stent can sometimes be placed to open affected blood vessels.
Surgery: In more severe cases, surgical options like hysterectomy with removal of the ovaries or surgical tying off of affected veins can be considered.
Lifestyle Changes: Managing weight, regular exercise, and avoiding long periods of standing can also help alleviate symptoms.
Compression Stockings: Wearing compression stockings can help reduce the discomfort caused by varicose veins in the legs, which sometimes accompany pelvic congestion syndrome.
Psychological Support: Because chronic pain can affect mental health, counseling or therapy might also be recommended to help cope with the condition.
Treatment decisions are typically made after a thorough assessment by a healthcare provider, often a gynecologist or a vascular specialist.
Pelvic Congestion Syndrome Treatment with Center for Vascular Medicine
In case your pelvic pain persists and does not respond or improve to typical treatments, it is recommended to see a vascular specialist. Center for Vascular Medicine provides specialized care and diagnostic services for patients dealing with pelvic congestion syndrome. Our team of experienced specialists is committed to identifying the root cause of your symptoms and developing personalized treatment plans. You can count on receiving unparalleled expertise and support throughout your treatment journey with Center for Vascular Medicine.
Contact us today to schedule a consultation and take the first step toward understanding and addressing your pain. We serve patients from Annapolis, MD, Columbia, MD, Easton, MD, Glen Burnie, MD, Greenbelt, MD, Prince Frederick, MD, Silver Spring, MD, Waldorf, MD, Fairfax, VA, Fredericksburg, VA, New Brunswick, NJ, and Union, NJ.

