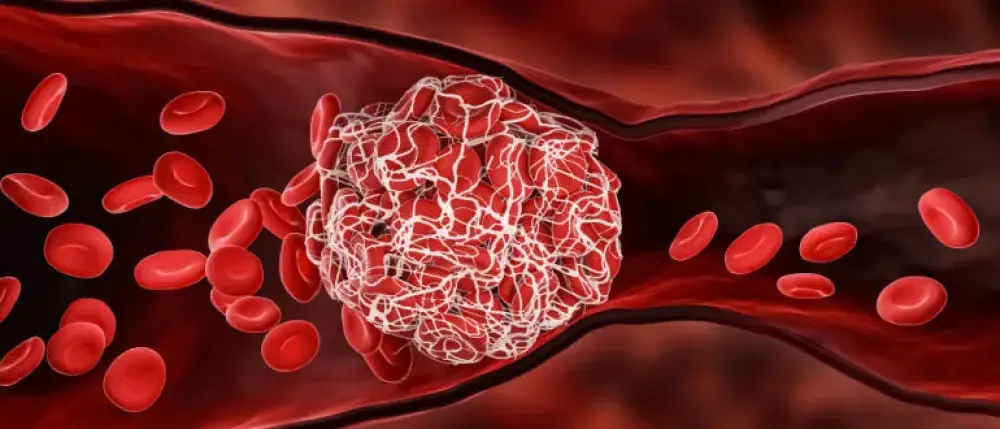
What Causes Blood Clots?
Blood clots can be more than a natural occurrence that forms when you get a cut or scrape. They can become a serious health problem and, if left untreated, can lead to severe complications. A blood clot forming within a deep vein can result in severe medical conditions. While blood clotting is a necessary process for wound healing and preventing excessive bleeding, it is essential to understand the risk factors, symptoms, and treatment options for DVT, which is a potentially life-threatening condition. Early detection and management of DVT are crucial to prevent serious complications.
Common Causes of Blood Clots
Deep-vein thrombosis (DVT), commonly known as a blood clot, occurs when a gel-like mass of platelets and fibrin forms in the blood to stop bleeding. If a blood clot forms incorrectly inside a deep artery or vein, especially in your leg, it can hinder blood flow and create further problems.
Common risk factors for a blood clot include:
Prolonged immobility: Sitting for long periods, such as during long flights or car rides, or being bedridden due to illness or surgery, can increase the risk of DVT.
Surgery or trauma: Major surgeries, particularly orthopedic surgeries like hip or knee replacement, can increase the risk of DVT. Trauma, such as bone fractures or severe muscle injury, can also contribute.
Advanced age: The risk of DVT increases with age, particularly over 60 years old.
Family history: A personal or family history of DVT or clotting disorders increases the risk.
Genetic predisposition: Inherited conditions that affect blood clotting, such as factor V Leiden mutation or prothrombin gene mutation, can increase the risk of DVT.
Obesity: Being overweight or obese puts extra pressure on the veins in the legs, increasing the risk of DVT.
Pregnancy: Pregnancy increases pressure on the veins in the pelvis and legs, increasing the risk of DVT, particularly in the third trimester and postpartum period.
Hormone therapy: Estrogen-based hormone therapy, including birth control pills or hormone replacement therapy (HRT), can increase the risk of blood clots.
Cancer and cancer treatments: Certain types of cancer and cancer treatments, such as chemotherapy or radiation therapy, can increase the risk of blood clots.
Chronic medical conditions: Conditions such as heart, inflammatory bowel, or lung disease increase the risk of DVT.
Smoking: Smoking damages blood vessels and increases the risk of blood clots.
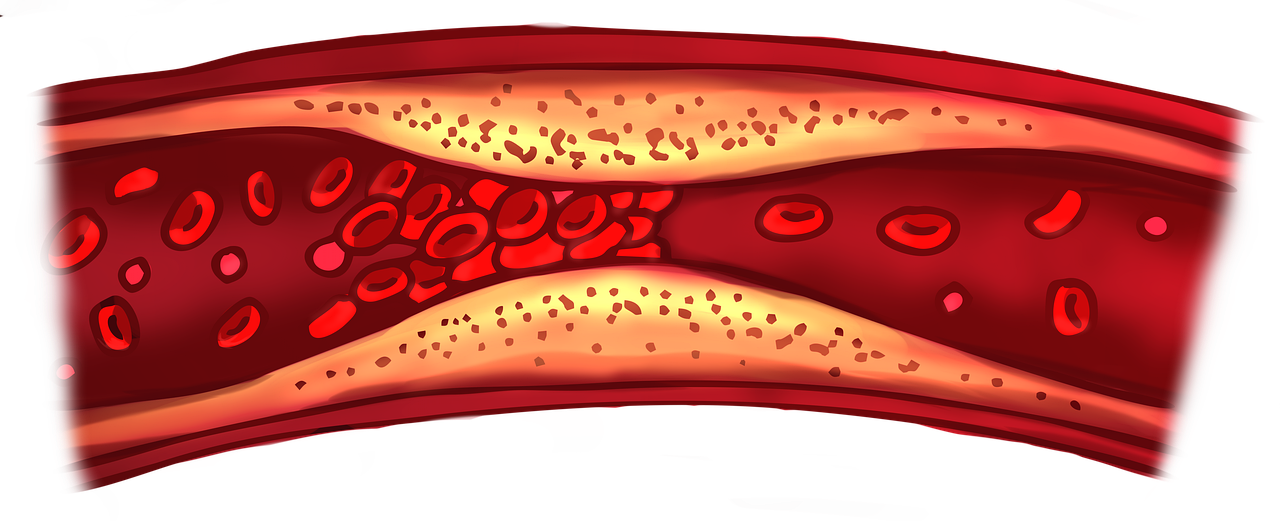
Varicose veins: Varicose veins can disrupt blood flow and increase the risk of blood clot formation.
Dehydration: Insufficient fluid intake can lead to thicker blood, increasing the risk of DVT.
Medication side effects: Some medications, such as certain types of antipsychotics or hormone treatments, can increase the risk of blood clots.
It's important to recognize these risk factors and take appropriate measures to prevent DVT, especially in individuals with multiple risk factors or a history of DVT.
If you suspect or discover there is a blood clot in your leg, you will need to get a professional diagnosis and decide on a treatment plan.
What are the Symptoms of a Blood Clot?
A DVT is a medical emergency. You should seek medical attention if you suspect you have the symptoms of a deep vein thrombosis.
The symptoms of a blood clot or DVT can vary depending on where the clot is located and its severity. However, common symptoms of a blood clot include:
Swelling: Swelling in the affected area, typically the leg or arm. The swelling may be accompanied by warmth and redness.
Pain or tenderness: Pain or tenderness in the affected area, often described as a cramp or soreness. The pain may worsen with movement or pressure.
Skin discoloration: The skin over the clot may appear red or discolored.
Warmth: The affected area may feel warm to the touch compared to surrounding areas.
Vein visibility: In some cases of superficial thrombophlebitis (a clot near the skin's surface), the affected vein may be visible and appear swollen and red.
Difficulty breathing: If a blood clot travels to the lungs (pulmonary embolism), it can cause sudden shortness of breath, chest pain, rapid heartbeat, coughing, and sometimes coughing up blood. This is a medical emergency and requires immediate attention.
Dizziness or fainting: A pulmonary embolism can cause dizziness, lightheadedness, or fainting.
It is crucial to seek medical assistance if you encounter any symptoms of blood clotting, particularly if you possess risk factors such as recent surgery, prolonged immobility, or a previous history of blood clots. Receiving prompt treatment can help prevent complications like pulmonary embolism or post-thrombotic syndrome.
How Will My Doctor Diagnose a Blood Clot or DVT?
Diagnosing a blood clot involves a combination of medical history, physical examination, and diagnostic tests. Here's how your vascular specialist will work with you to determine if a blood clot causes your symptoms:
Medical history: Your doctor will ask you about your symptoms, medical history, and any risk factors you may have for blood clots. They will inquire about recent surgeries, injuries, travel history, and any family history of blood clots or clotting disorders.
Physical examination: Your doctor will perform a physical exam focusing on the affected area. They may check for swelling, redness, warmth, and tenderness in the legs, arms, or other areas where a blood clot is suspected.
Blood tests: Blood tests can help diagnose blood clots or determine if you have an underlying condition that increases your risk of clotting. Standard blood tests include the D-dimer test, which measures a substance released when a blood clot breaks up, and clotting factor tests, which evaluate your blood's ability to clot.
Ultrasound: Duplex ultrasound is a standard imaging test used to diagnose blood clots in the legs (deep vein thrombosis). It uses sound waves to create images of the blood vessels and can detect blood clots and evaluate blood flow.
Venography: Venography involves injecting a contrast dye into a vein, usually in the foot or ankle, and then taking X-ray images to visualize blood flow and detect any blockages caused by blood clots. It's less commonly used than ultrasound but may be necessary sometimes.
The diagnostic tests for blood clots depend on your symptoms, medical history, and suspected clot location. Early diagnosis and treatment are crucial to prevent complications.
What’s the Treatment for Blood Clots?
Your medical team will recommend the best course of treatment for you based on your medical history, the location of the clot, and your test results.
The most common treatment for a blood clot is anticoagulants or blood thinners. They reduce the body's ability to form new clots and prevent existing clots from growing larger. Anticoagulants can be given as pills or intravenous injections. Some individuals may take them only for the duration of the clot or longer to prevent new clots from forming.
Regularly monitoring and adjusting the dosage of anticoagulant therapy is crucial to ensure its effectiveness while minimizing the risk of bleeding complications. This often requires routine blood tests to assess the medication's impact on clotting factors and adjust dosages accordingly.
Thrombolytics are medications for individuals with blood clots that haven't responded to standard anticoagulants or in cases where the clot burden is extensive and poses an immediate risk. These dissolve blood clots but can increase bleeding risk. Administered through a catheter or injection, they're used in severe situations where vital organs or tissues are at risk due to a large clot or impaired blood flow.
Surgical thrombectomy is rarely necessary for a blood clot. Seek early treatment to avoid surgery. It is considered a last resort due to risks such as bleeding, infection, and anesthesia-related complications. Only some people qualify for surgery, depending on their health condition and the clot's location.
What’s My Prognosis After DVT Treatment?
Most patients who seek out medical care in a reasonable amount of time recover within several weeks or months of treatment without any complications. With appropriate treatment and management, the majority of individuals with DVT can expect a good prognosis with resolution of symptoms and a reduced risk of complications. It’s important to continue following up with your Center for Vascular Medicine vascular specialist as directed to monitor for any potential complications or recurrence of the condition. Your healthcare provider can provide personalized prognosis guidance based on your medical history and circumstances.
Exceptional Care for Vascular Conditions at the Center for Vascular Medicine
At the Center for Vascular Medicine (CVM), we are committed to providing top-notch and compassionate care for people with vascular diseases. Our team of experts focuses on venous and arterial conditions affecting the legs, feet, and pelvis. We are dedicated to crafting personalized treatment plans tailored to your needs.
Our board-certified vascular specialists offer personalized care with advanced ultrasound scans to diagnose vascular diseases, including blood clots and deep vein thrombosis. Our experienced specialists identify the root cause of your symptoms and develop targeted treatment strategies. You can expect unmatched expertise and support at every treatment step with Center for Vascular Medicine.
Schedule an appointment today at one of our Maryland, Virginia, or New Jersey locations.
Ready to speak with a vascular specialist?
FAQs
While there are no natural remedies that can directly dissolve blood clots, some lifestyle changes can help reduce the risk of developing DVT. These include regular exercise, maintaining a healthy weight, quitting smoking, and avoiding prolonged periods of sitting or standing.

